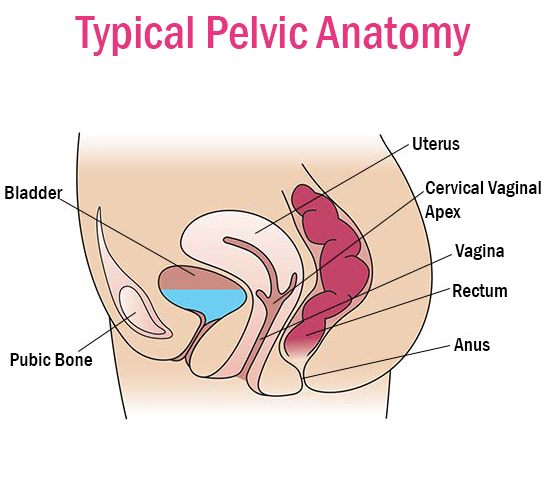
Prolapse affects approximately 40 percent of women, to some degree, and can be caused by vaginal childbirth, prior surgery and repetitive coughing or straining. It is further exacerbated by low estrogen resulting from menopause. It occurs when there is weakness or damage to the normal support of the pelvic floor, which holds up the pelvic organs. If the muscles of the pelvic floor and layers of connective tissue, which are called fascia, become weakened, stretched, or are torn the pelvic organs may fall downward. In severe cases, women may feel or see tissue coming out of the opening of their vagina. This can worsen over time.
The Female Pelvic Health Center offers treatment options for many types of pelvic organ prolapse.
Visit the Association for Pelvic Organ Prolapse Support for more information and resources.
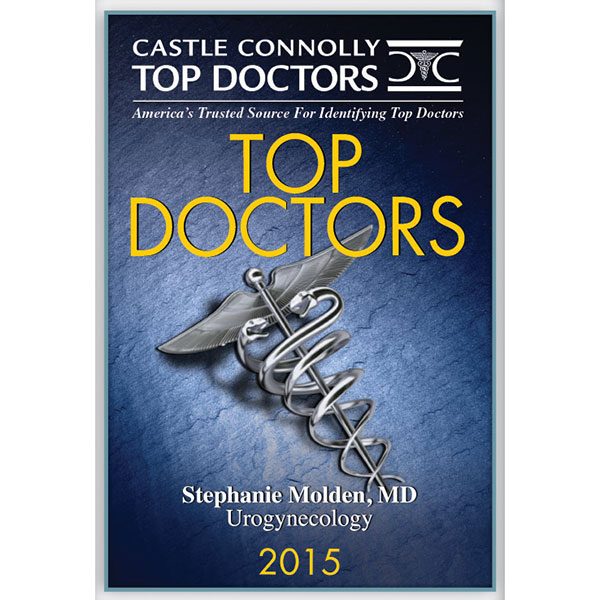
Cystocele Prolapse
Also known as Dropped Bladder or Anterior Prolapse, occurs when the supportive tissue between a woman's bladder and vaginal wall weakens and stretches, allowing the bladder to bulge into the vagina. Straining the muscles that support your pelvic organs could lead to this condition. Such straining occurs during vaginal childbirth or with chronic constipation, violent coughing or heavy lifting. This also tends to cause problems after menopause, when estrogen levels decrease. For mild conditions nonsurgical treatment is often effective. In more severe cases, surgery may be necessary to keep the vagina and other pelvic organs in their proper positions.
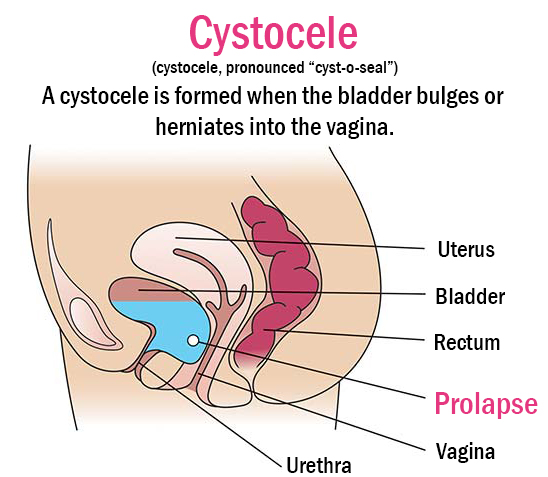
Uterine Prolapse
Uterine Prolapse is a condition when a woman's uterus sags or slips out of its normal position. The uterus is held in place by a group of muscles and ligaments. Several factors can contribute to the weakening of these muscles and ligaments, causing the uterus to sag. These factors include the loss of muscle tone as women age, injury due to childbirth (especially women who have had many babies or large babies), obesity, chronic coughing and chronic constipation. Any of these factors can place added tension on the pelvic muscles. While mild cases of uterine prolapse often have no symptoms, more severe cases can actually interfere with bowel, bladder, and sexual functions.
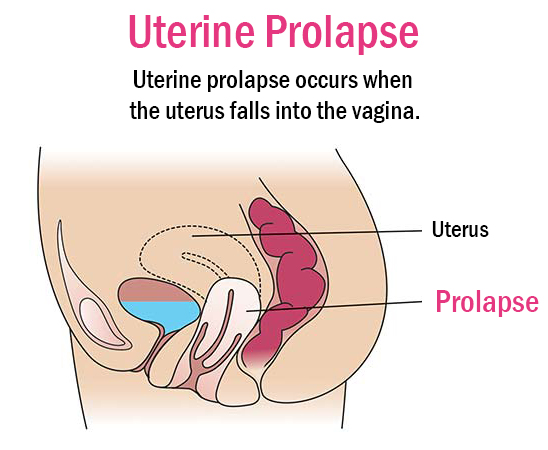
Vaginal Vault Prolapse
Vaginal vault prolapse occurs when the upper portion of the vagina loses its normal shape and sags or drops down into the vaginal canal or outside of the vagina. Vaginal Vault Prolapse is usually caused by weakness of the pelvic and vaginal tissues and muscles. It happens most in women who have had their uterus removed in a hysterectomy. Symptoms include pelvic heaviness, backache, vaginal bleeding and a mass bulging into the vaginal canal or out of the vagina that may make standing and walking difficult.
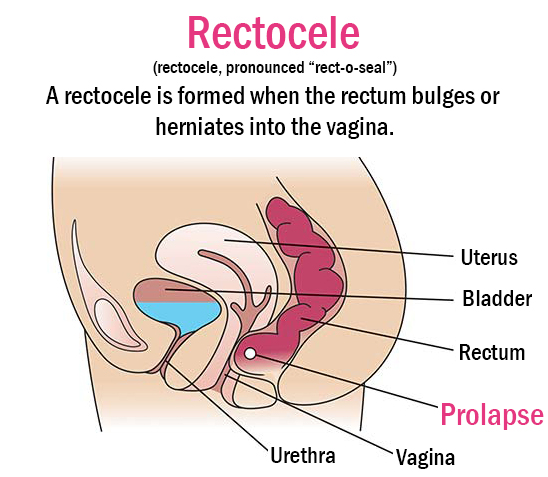
Rectocele Prolapse
Also known as Rectum Prolapse, occurs when there is a break in the supportive layer of the vaginal wall. When there is a loss of support, the rectal wall will come into contact with the vaginal skin and create a bulge. The bulge will usually increase in size with bearing down, especially when having a bowel movement.
Also called small bowel prolapse, this occurs when the small intestine (small bowel) descends into the lower pelvic cavity and pushes at the top part of the vagina, creating a bulge. Childbirth, aging and other processes that put pressure on your pelvic floor may weaken the muscles and ligaments that support pelvic organs, making enterocele prolapse more likely to occur. Mild enterocele prolapse may produce no signs or symptoms. However, if you have significant prolapse, you might experience a pulling sensation in your pelvis that eases when you lie down, a feeling of pelvic fullness, pressure or pain, low back pain that eases when you lie down, a soft bulge of tissue in your vagina or vaginal discomfort and painful intercourse (dyspareunia).
To manage this kind of prolapse, self-care measures and other nonsurgical options are often effective. In severe cases, you may need surgical repair.
Treatment Options
Click for more information.